I got Sucker Punched by Workplace PTSD, How About You?
As we enter Horticultural Therapy (HT) Week, I feel like it's important to bring a bit of awareness to a safety issue that may not be on your radar, Workplace PTSD.
Working with plants has so many innately therapeutic benefits that a lot of other careers lack. But, one thing that I’ve learned over the last few years is that no one, and no profession is immune to Workplace PTSD. Now, I know what you may be thinking, “PTSD seems extreme”, Or perhaps, “this stuff sounds kind of whingey, no one likes work”. But did you know that having someone humiliate you sends the same chemicals rushing through your body as a punch in the gut? And, if those systems are activated daily, your body will experience serious disfunction that you cannot control?
“While the concept is widely recognized in military personnel, combat veterans, and victims of assault, the truth is that PTSD can and does affect people who have encountered trauma in a huge variety of settings — including the workplace.” (Carla M. Manly, clinical psychologist)
For too long we've accepted violence, abuse and harassment as part of our working lives. Something that is upsetting but happens; it's a given. And yet It doesn't have to be this way, we can choose not to accept it. There is no reason for co-workers, supervisors, clients or members of the public to act in an abusive way in any place of work. These behaviours have very real and longterm consequences and costs.
Please note that I'm not a health care professional (I'm a Horticulturalist) so I won't be diving into the clinical descriptions and diagnosis' of PTSD. Instead, I'm looking to share some of the information and experiences that I've collected over the years in the hope that we can raise awareness and initiate open conversations. That will in turn, lead to meaningful changes in how we see our occupations and how they effect our health.
“Anyone can experience a trauma. Why some people are more impacted than others is complex. It often depends on their age, their ability to tolerate uncomfortable feelings, and [whether they have] supportive relationships with family and friends. All these factors impact our ability to cope.” (Kelly Kellerman, Thriveworks)
A Bit of My Story
It’s something that I’d never even considered happening to me…until it did. I started a job that I thought might be really cool (not to mention financially necessary). And, I was pretty happy until little things began to creep in.
Everyday started with a meeting, where my supervisor would address our crew in an area shared by a half dozen other groups. And you never knew what you were going to get. More often than not, he would approach like a cinematic drill Sargent. Demanding attention, yelling orders, changing tasks for no apparent reason and if anyone questioned him, there was always a loud demeaning response and punishment meted out. But it was ok, because “that’s just how he is, and if you don’t like it you can leave”.
It wasn’t all bad, our crew learned to support each other behind his back. A knowing look, a pat on the shoulder or maybe, “don’t worry, it’ll be someone else’s turn next week”. We would get our work done in spite of it.
He knew where the line was, he only made comments, gossiped or laughed behind his targets backs with colleagues that encouraged him (or at least failed admonish him). He physically intimidated without making contact. Blamed others for the damage his temper caused to equipment and tools. The mechanics would joke about his predation on new female employees. Other crews would giggle nervously when he induced so much anxiety in someone that they caused an accident or made a mistake. Colleagues from other departments would say, “oh it can’t be that bad, or someone would do something about it”. It was accepted that the behaviour was ok and that we should all grow a tougher skin in response.
I watched as he targeted those who spoke up. Micro aggressions when others were around and derogatory names and yelling when we were out of ear shot. My rheumatoid arthritis flared and I dropped out of a five year remission. One coworker started eating more, he said he was drinking too much and felt angry all the time. Another withdrew, rarely showing up for shifts and when she did, was jumpy and willing to do anything to avoid a confrontation (including spreading rumours to shift attention away from herself). Another retired early, having developed an auto-immune disease after years of depression and thoughts of self harm. The stress and trauma affected each crew member differently, but no one went unscathed. I watched friends who loved their profession lose their spark and shrink away until they either quit or resigned themselves to a depressive state.
Anyone who sought help from our union, Hr department or those who weren’t affected by a power imbalance hit a brick wall. There was a blatant disregard for anything that didn’t fit the narrative that they wanted, most especially if it looked like it might cause them a PR problem. Confidential information was leaked, any actions taken were minimal and easily laughed off. Incidents were ignored until they escalated to a point where people were fired. But, the culture never changed.
After a dozen years of this behaviour (plus additional discrimination, sexism and more), I struggled to shake it off as easily as I once did. I found that I was being triggered by small things (the sound of a particular truck or a ringtone). I started throwing up before the morning meetings and, I felt a car hit me, if I saw someone from work in my private life (particularly if it was unexpected). My behaviour at work shifted from light-hearted banter to guarded angry silence. And, I couldn't control any of it.
Finally, I couldn’t ignore it anymore. All of the thousands of small stressors had had a cumulative effect that was so much greater than the sum of its parts. I felt like I needed to follow the in-flight card and put on my own oxygen mask before I helped others, so I walked away. The only thing that I regret, is not leaving sooner. But I’d never experienced these symptoms before. I honestly thought that I could brush off the behaviour and push through somehow; continue on my chosen career path. It took me some time (with some professional help) to really understand what had happened to me.
I now run my own business. My RA returned to remission 6 months on from my departure and I learned to spot and rewire my triggers (neuroplasticity is amazing). My perspective on work has also evolved to include a greater awareness of others; not only watching for abusive behaviour but also for those that may be experiencing PTSD without realizing it.

Common Toxic Behaviours
Manipulation and Harassment (in addition to sexual and racial)
undelivered promisses
boundary violations
not allowing you to use sick or vacation time
purposely creating instability (changing planned tasks, times or placements for no reason)
physically intimidating
Aggression and Emotional Abuse
dressing down subordinates in front of colleagues
pushing workers to perform tasks they aren’t trained for
purposely disregarding safety protocol
requiring availability and responsiveness at all times, including outside of work
unrealistic performance expectations
not being given the resources to succeed
being overly critical or judgmental
Discrimination
being singled out for things that don’t effect work performance (physical differences, race, religion, orientation etc)
pushed to do unnecessary assessments
given ‘help’ that wasn’t requested (different tools, equipment or altering tasks)
In other words, behaviours that leave workers feeling that they aren’t psychologically safe at work.

Trauma Responses
Did you know that verbal attack can cause the same response in your body as a punch in the gut?
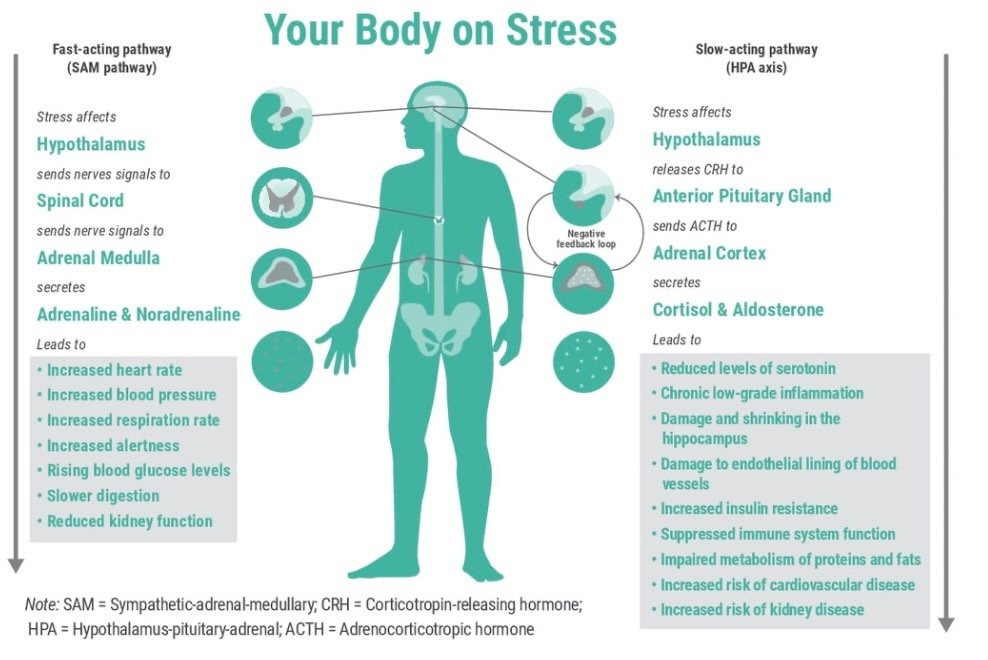
When your brain receives stimulus it activates two unique paths to help your body react, the HPA axis and the SAM axis. In a highly stressful situation, whether physical or psychological, the brain is hardwired to override it's normal responses. Instead within milliseconds, a cascade of hormones is triggered (by the SAM axis) producing immediate physiological changes (aka the ‘fight or flight’ response). The SAM axis,
floods adrenaline through the bodies systems
increasing blood flow to your heart and muscles
muscles tense to guard against pain and injury
oxygen intake increases
Simultaneously, the HPA releases it's own hormones like cortisol. Shutting down any unnecessary systems (motor skills, immune system, reproductive system, including healing and digestion). Rerouting it's resources to give the body a better change of survival. It,
increases energy, muscle strength, mental alertness and vigilance
heightens glucose levels and retention of sodium (for increased short term energy)
In Workplace PTSD these responses get stuck in a loop, never reaching recovery. And eventually, prolonged exposure prompts long-term dysfunctional responses. Altering the normal functions of the HPA axis, changing how susceptible we are to trauma in the future.
General Adaption Syndrome categorizes these changes. Separating them into three stages, with the last two showing the pathological issues resulting from extended stress (aka Workplace PTSD).
The alarm reaction stage, is that initial "fight or flight" response we spoke about.
Then as the trauma passes, the body decreases the cortisol levels slightly (lowering heart rate and blood pressure etc), in order to begin the recovery process. While also keeping the body on alert, in case the threat returns. If this state persists for an extended time, the body then adapts in order to cope with the situation. It continues to release cortisol, locking the body in this state of alert. This causes the resistance stage, where we start to see symptoms of poor concentration, irritability, and more.
If the stressful events continue to remain unresolved, the body then enters the exhaustion stage. This is when the body reaches burnout, fatigue, depression, anxiety, and reduced stress tolerance. It's like a speaker thats dial is broken. When you power it up, the volume starts at 11 and only climbs higher. In other words, a small stressor then elicits a huge reaction.
Eventually, the continued suppression caused by stress hormones will weaken the bodies immune system causing long-term medical issues.
Signal and Response
Triggers can include;
workplace noises (ringtone, email, truck)
traveling your regular commute
certain places
banal conversations (really)
Any of the specific places, people, or situations where you might have encountered trauma in the past. It's your bodies way of warning you that danger is present.
Symptoms can surface as;
chest pains
nausea and vomiting
muscle spasms
jitters
chronic anxiety
panic attacks
apathy
depression
hopelessness and despair
withdrawal
persistent negative and intrusive thoughts
suicidal ideation
hyper-reactivity
exhaustion
emotional numbing
self-isolation
sleep difficulties
lack of focus
memory loss
irritability
negativity
avoidance of work
self-blame
blaming of others
flashbacks

Employer Response
An employers response to an instance of Workplace PTSD can have a huge impact on the health and recovery of those effected. Staff should treat suspected cases as a serious condition, listen to employee concerns about feeling unsafe and seek to reduce or remove stressors that may be causing trauma. It’s a complex issue that will likely require individual investigation and treatment in each instance.
“It’s important for HR staff to know that genetic, environmental, personality, and historical elements all contribute to a person’s propensity for developing PTSD. For example, if two people are exposed to the same experiences in a hospital setting, one may develop PTSD and another may not.” (Carla M. Manly, clinical psychologist)
There are many ways to show support and encourage recovery. The most important include actively listening with compassion and an open mind, investigating and then taking appropriate and specific actions. Always following policies with consistency and clarity in order restore the sense of safety not only for those directly involved, but also as a piece of the greater workplace culture and morale.
Workplace PTSD is not a weakness or a personal problem. Rather, it can be seen as an indicator of employee phycological safety issues in a similar way that a workplace injury may speak to physical safety standards in place. In fact, I would suggest that just as an injury triggers a safety investigation, so should an instance of Workplace PTSD.
Besides implementing policies, protocols and guidelines to ensure worker safety, employers can also provide tools (access to benefits for counselling and treatment services) to members of their workforce. Employers don’t have to provide therapy, rather offer an open and safe place to talk. The decision to seek professional treatment is up to the employee, in the same way that a physical injury is.
Colleagues and Employers Should Watch for;
absenteeism
low morale
high turnover
early retirement
increase in accidents, errors
change of personality
change in performance
physical health complaints
social withdrawal
erratic behaviours (angry outbursts)
increased conflict
increase in substance use
poor career decisions

Recovery
If you are experiencing any signs or symptoms of Workplace PTSD, or know someone who is, it’s always best to seek professional help. It’s important that you tell someone what you are experiencing, just as you would for a broken bone resulting from a workplace accident. Report instances to your employer and local authorities (occupational safety groups, employment insurance agencies etc). Additionally, friends, family, coworkers and other groups can all offer support, and help to find solutions to aid recovery.
It also helps if you’re able to make use of any protocols and systems that employers may have in place. However, you should always be aware that many corporations, HR departments and unions have a propensity to look after their own interests first (so keep your critical thinking cap on). Be sure to prioritize your own health and find an appropriate advocate that specifically represents your personal needs. Remember that being healthy is so much more important than any job. You are not alone, help is out there and recovery is real.
Horticultural Therapy is a highly successful avenue of treatment as part of multi-disciplinary clinical program. You can find more information, locate HT practitioners, or get HT career advice through your national HT Association (CHTA, AHTA, ThriveUK). Therapeutic Gardening/Horticulture can be a great support as well, in a less clinical instance. So get gardening and don't forget to check with your local healthcare facilities and associations for HT/TG meet ups and programs in your area. They’re great for making social connections, learning new things and having some planty fun.
Sara-Jane at Virens Studio
Virens is a studio located in Vancouver, Canada. We specialize in ecological landscape and planting design (including therapeutic gardens) and urban greening. Offering plans, consultation and also freelance writing services. In addition to our site, visit us on IG and Substack.





What a great and informative article. Thank you Sara-Jane.